Ten-Year Outcomes and Risk Factors After Anterior Cruciate Ligament Reconstruction: A MOON Longitudinal Prospective Cohort Study.
MOON Knee Group, Spindler KP, Huston LJ, Chagin KM, Kattan MW, Reinke EK, Amendola A, Andrish JT, Brophy RH, Cox CL, Dunn WR, Flanigan DC, Jones MH, Kaeding CC, Magnussen RA, Marx RG, Matava MJ, McCarty EC, Parker RD, Pedroza AD, Vidal AF, Wolcott ML, Wolf BR, Wright RW. Am J Sports Med 2018. 46(4): 815-825.
https://www.ncbi.nlm.nih.gov/pubmed/29543512
Take Home Message: After an anterior cruciate ligament (ACL) reconstruction, patient-reported outcomes increase during the first 2 years and then are maintained at 6 and 10 years post-surgery. A participant who at the time surgery had a higher BMI, medial meniscus procedure performed prior to reconstruction, female sex, older age, smoking habit, chondral lesion, or poorer patient-reported outcome scores were more likely to have inferior outcomes at 10 years.
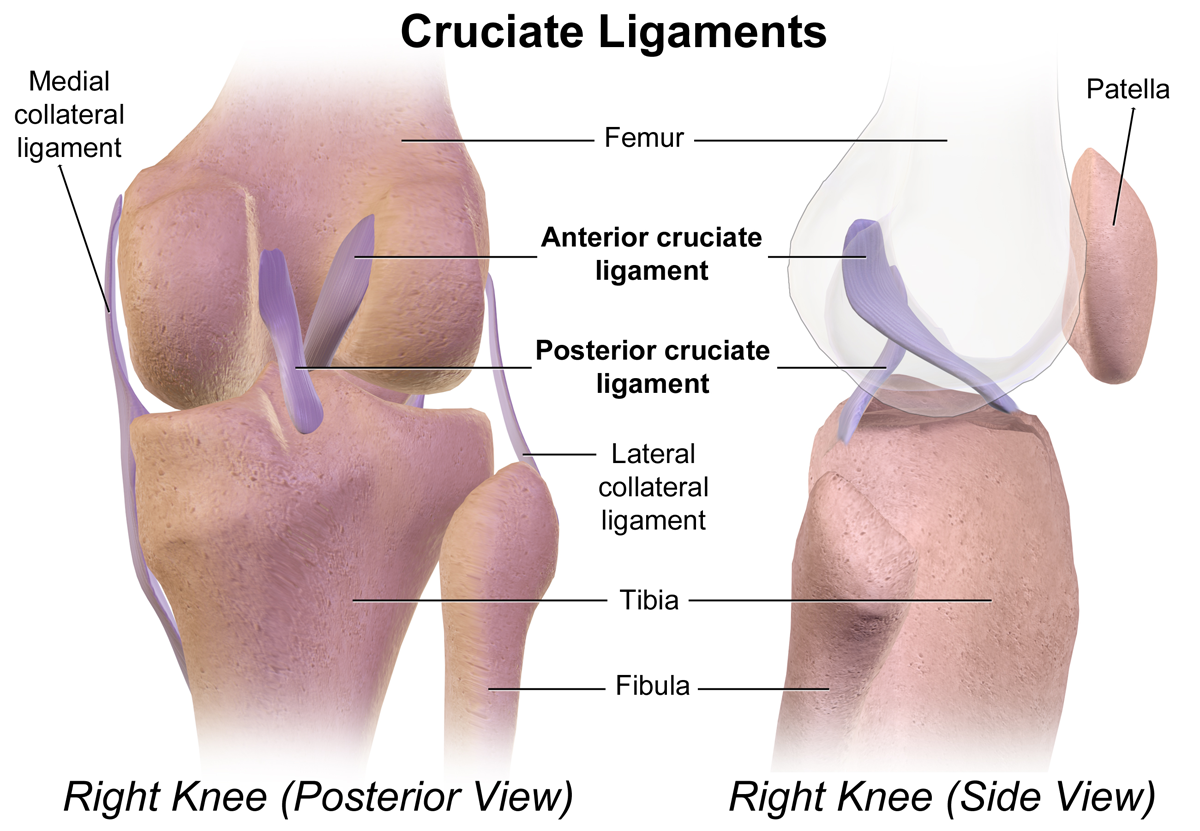
Anterior cruciate ligament (ACL) rupture is a common injury in sport that can lead to long-term degenerative joint changes and greatly affect an athlete’s short- and long-term quality of life. However, few studies have followed patients long after an ACL reconstruction to find out how they are doing and what factors are related to inferior outcomes. Therefore, the MOON Knee Group completed a prospective study to identify risk factors for inferior outcomes 10 years after an ACL reconstruction. A total of 1592 patients who had a primary or revision ACL reconstruction at 1 of 7 sites in the consortium were enrolled in the study. All patients completed informed consent, and a 13-page questionnaire, which included the International Knee Documentation Committee (IKDC), Knee Injury and Osteoarthritis Outcome Score (KOOS), and Marx activity rating scale score. All patients underwent a standardized rehabilitation protocol after surgery. The same questionnaire that was issued at enrollment was re-issued via mail at 2, 6, and 10 years post-surgery. The authors obtained 10-year follow-up data from 83% of participants. On average, participants reported improved outcomes (IKDC and KOOS scores) from surgery to the 2-year follow-up and these improvements were maintained at the 6 and 10-year follow-ups. In contrast, the participants’ activity typically decreased over time. Overall, a participant who started with a higher BMI, medial meniscus procedure performed prior to reconstruction, female sex, older age, smoking habit, chondral lesion, or lower patient-reported outcome was more likely to have an inferior outcome. Level of activity, graft type, medial collateral ligament or lateral collateral ligament lesions, and meniscus lesions at the time of reconstruction were not significant factors.
Overall, these findings highlight that on average people perceive improvements from surgery to 2-years and then maintain these results overtime. It would be interesting to know how people individually changed. For example, how many people continued to have meaningful improvements over 10 years versus how many had meaningful declines in quality of life or function? In the meantime, clinicians can use these results to counsel patients. It may be beneficial to discuss with patients the modifiable risk factors (e.g., smoking, high BMI) that the authors identified and what they mean to a patient if they have one. These factors such as lower baseline activity scores, high BMI, and being smoker, can be targeted by clinicians as behaviors that can be modified even before an injury occurs. As clinicians gain a better understanding of the factors that can lead to the best outcomes, more detailed and efficient surgical procedures, rehabilitation programs and pre-injury intervention programs could be identified and implemented. In the meantime, clinicians should continue using their current treatment protocols but should consider counseling patients on these modifiable factors both before and at the time of injury.
Questions for Discussion: Are the modifiable factors which you council athletes or patients on prospectively? If so, how did you previously identify those factors and are they consistent with those in this study?

Thank you for sharing this article! I have never thought about patient demographics being a risk factor for poor outcomes after an ACL reconstruction. I have always focused on quad strength and ROM as the main factors that can effect outcomes. Although, working with Division I athletes, smoking and high BMI are rare demographics for them, I do encourage them to meet with our sports nutritionist to create a plan to maintain weight through rehab. As I move forward in my experiences, I will definitely keep these risk factors in mind and advise my patients accordingly.
Kim, thanks for the great comment. I agree that some of these demographics might be less common for athletes but it can help put the clinician in a good frame of mind which is to think about modifiable risk factors before the injury occurs. It’s also wonderful to hear that your position provides your athletes with other professions who could help them enact the changes necessary to improve outcomes.